Good Afternoon!
You might remember my iron overload saga. Back in October, I discovered I had functional iron overload. Too much iron in the body is actually a pretty common problem. Too much iron causes oxidative damage in the body. For me, this was causing depression, insomnia, food sensitivities, knee pain, muscle pain, shoulder pain, hormonal issues, and difficulty concentrating (among others I can’t remember right now). The treatment is to give blood, which I have done a few times.
I gave blood again last Friday. Yesterday I got the email reporting my cholesterol (a nice bonus for people who give blood at the Miller-Keystone blood bank). Now, this is interesting:
- On 11/16/2018, my total cholesterol was 249. My blood pressure was 127/84.
- On 1/25/2019, my total cholesterol was 197 and my blood pressure was 115/72.
I also had blood pressure taken back in October the first time I gave blood and it was a little high (I can’t remember the exact number, and that was at LGH, where they don’t provide the historical data).
Of course, one can’t draw generalized conclusions from the example of one person and only two data points HOWEVER I can report the fact that the only thing I changed was to give blood a few times and both my cholesterol and blood pressure went down. Giving blood does have documented benefits: it can lower LDL-c, total cholesterol, and blood pressure, improve glycemic control, and may help prevent atherosclerosis. Along with the other beneficial side-effect of saving lives 😊
I can also say I’m happy I didn’t panic when I saw that 249 cholesterol number. People can easily panic when blood numbers look off and end up on drugs *shudder*. For me, it would have been completely unnecessary.
(Side note—I’m going to write more about cholesterol soon, but in short, the causes are metabolic disease/sugar handling problems, thyroid issues, and oxidative damage. In my case, my cholesterol was going up due to oxidative damage from too much iron.)
Now let’s get back to looking at how food sensitivities can mimic Lyme disease symptoms.
Food sensitivities (not to be confused with true food allergies) are on the rise. There are a lot of hypotheses as to why this might be. Changes in gut flora perhaps, affected by widespread antibiotic use, increased prevalence of c-section and infant formula? The widespread use of the herbicide glyphosate (that kills good bacteria too, by the way)? Maybe increasing amounts of GMOs in the food supply?
Even though no one knows why so many people have food sensitivities, just ask any health practitioner and they will tell you—it’s getting worse. Patients report symptoms such as fatigue, brain fog, joint pain, headaches, migraines, skin rashes (e.g. eczema), stomachache, acid reflux, bloating, constipation, diarrhea, weight gain, weight loss, and behavioral issues (in children). Many of these effects are not immediate but can occur several days after ingesting the offending food. Notice how many of these food sensitivity symptoms overlap with symptoms of Lyme Disease.
The most common foods implicated in food intolerances are wheat, dairy, hen’s eggs, soy, grains, nightshades, yeast, citrus, and legumes. Some of these intolerances are immune-mediated; many are not, being caused by other factors. As clinicians, we are not as concerned with the exact cause or mechanism of the reaction to the offending food. We are more concerned with the strategies that will get people results.
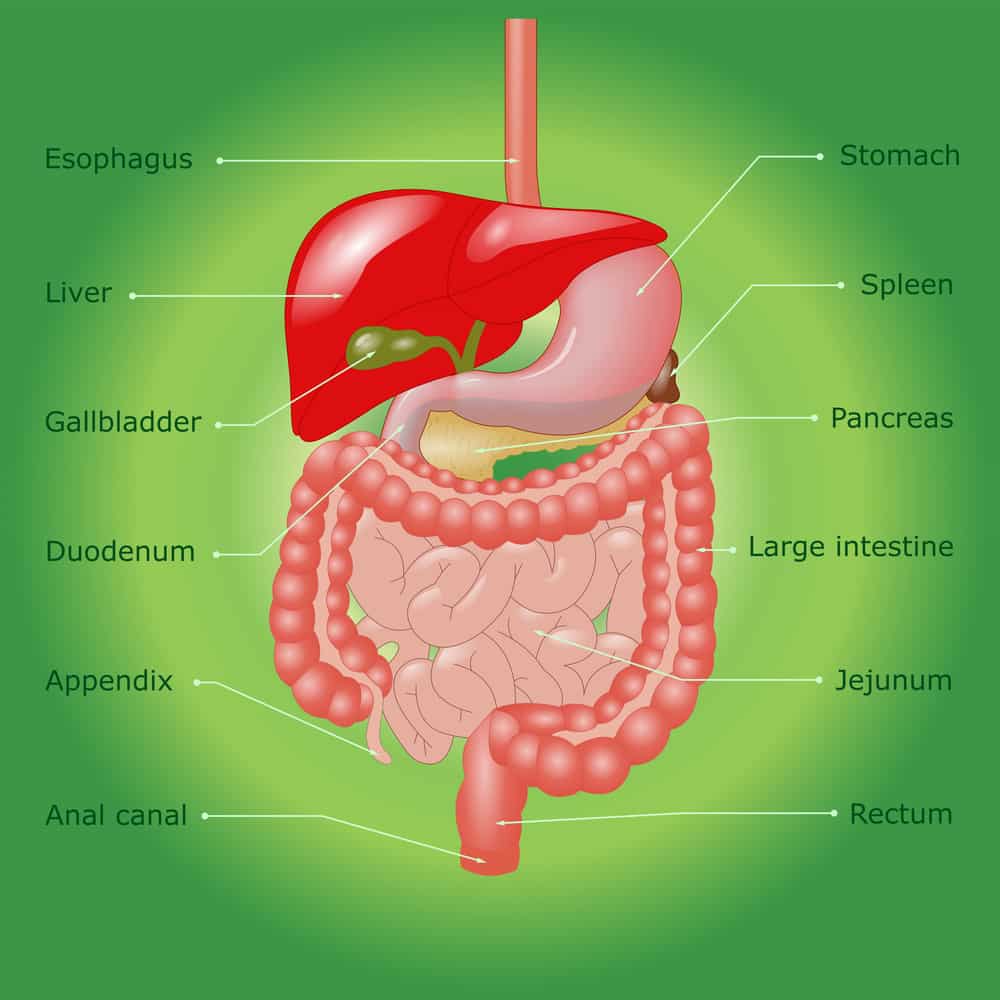
Both Dr. Sheehan and I have seen people who thought they had Lyme Disease, but actually food intolerances were causing all their problems. Whether Lyme Disease is present or not, people most often will not get better unless they remove the offending food(s) from their diet. The next step is providing some help to a gut in need of healing! This can be accomplished through Nutrition Response Testing and Functional Medicine by identifying the organ weakness(es) and providing the appropriate nutritional support. Common organs needing some help are the liver, gall bladder, small intestine, pancreatic enzyme production, and stomach acid production.
Diet-wise, we have found that a Paleo Reset works great, as most problematic foods are automatically excluded. People will find their energy improves and digestive issues will clear up. Skin will also often improve. Without foods that are toxic to your body holding you back, your immunity will also get a serious boost (bonus for people with Lyme Disease)! Check out this video from a patient who just reversed his diabetes (spoiler—all he did was cut out gluten), and another patient here lost 10 lbs. in 8 days so IT CAN BE DONE, PEOPLE!
Nutritiously yours,
Laura Sheehan