November 21, 2019
When Donna came in to see me early this year 2019, she was complaining of digestive issues, chronic sinus problems, and fatigue. She had been to see several doctors over the years but hadn’t gotten much relief. Notably, she had had surgery for endometriosis in 1989, part of her bowel removed in 2016 and had her gallbladder removed in 2001. Something didn’t add up. I knew that Donna took good care of herself and had worked with nutritional doctors in the past. But she still wasn’t feeling well. And I knew that she had a great diet, yet she still had a lot of digestive discomfort and pain, fatigue and sinus issues.
Considering all of this, I asked to see her most recent labs. Notably, and shockingly, no one had performed an iron panel, thyroid panel, or even a vitamin D level! Fail! So I ordered these for Donna. To show the difference between functional medicine values and standard lab reference ranges, I decided to show you the two of them.
| Marker | Value | Functional Range | Lab Range | ||
| TIBC | 279 | 275 – 425 | 250 | – | 450 |
| UIBC | 141 | 175 – 350 | 150 | – | 375 |
| Iron | 138 | 40 – 135 | 40 | – | 155 |
| Iron saturation | 49 | 17 – 45 | 15 | – | 55 |
| Ferritin | 329 | 30 – 200 | 15 | – | 150 |
| TSH | 1.51 | 0.5-2.0 | .45 | – | 4.5 |
| T4 (Total) | 6.7 | 6.0-12 | 4.5 | – | 12 |
| T3 Uptake | 23 | 30-38 | 24 | – | 39 |
| Vitamin D, 25-OH | 24.6 | 35-60 | 30 | – | 100 |
As you can see, using the standard lab reference ranges (highlighted in red) she has high ferritin, low T3 uptake, and low vitamin D. In other words, she has high iron (or inflammation), a little bit of thyroid stress, and low vitamin D. But, using the functional medicine reference ranges (in blue), you can see that Donna’s big problem is that she actually has iron overload! Wow!
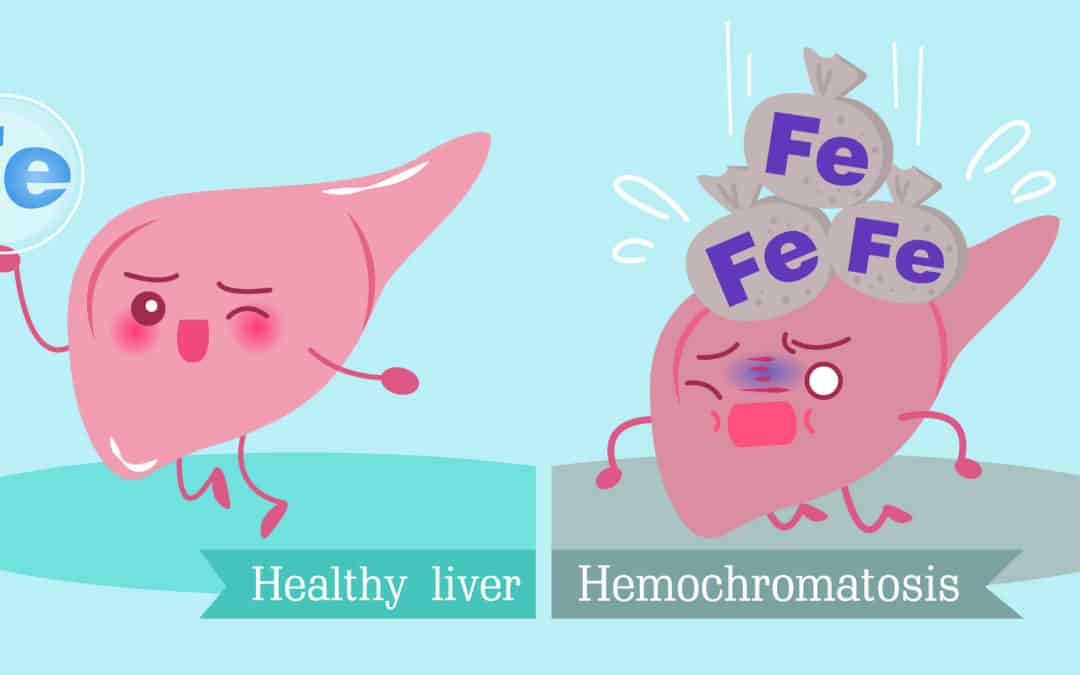
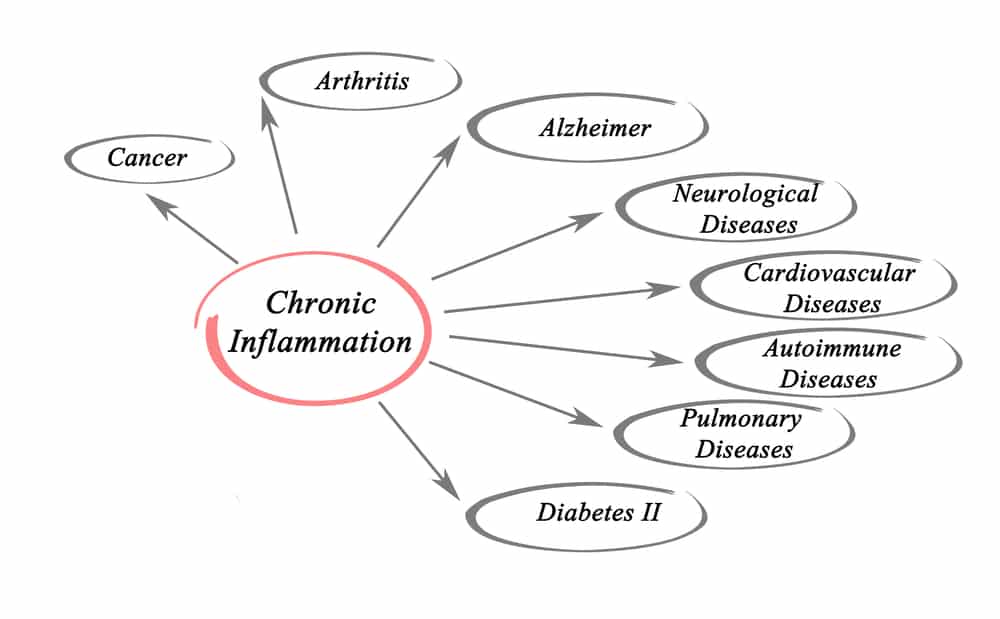
This would account for a lot. You see, iron overload is actually quite common, affecting between one and nine, and one in three people in this country. Common signs and symptoms of iron overload are joint pain, fatigue, depression, as well as increased risk of heart disease, high blood pressure, cancer, Alzheimer’s, Parkinson’s, diabetes and other diseases. Personally, in my office, I see that it is usually also associated with digestive problems and immune system issues, such as chronic sinus problems.
Excess iron in the body tends to accumulate in the liver, heart, blood vessels, brain, and nerves. It’s kind of a big deal! Could this actually be a root cause of Donna’s problems? Well, it bears ruling out. What is the treatment for iron overload? This is probably one of the most obvious reasons why you never hear of it—the treatment for iron overload is free! Just give blood! Not only is it free to give blood, but you get to help another human being that needs it! Win!
Donna followed through with my recommendations, with a small supplement program that supported her digestive tract and immune system, while giving blood. Within a couple of months, she was virtually symptom-free! Another win!
Fast forward to last week. I had not seen Donna since May, and since I am writing an article about her case, I decided to call her. She confided in me that she had not given blood in several months and that she was severely stressed taking care of her elderly father, who just passed away. I asked her “Did you feel better when you followed the program and gave blood?“ She replied, “Oh yes, I felt much better, but I have not been able to keep up with everything because I was taking care of my father these past months, I intend to get right back on the program and feel better again! “
So why is this so important? Why am I blogging about this specific case? One, I’m blogging about this to tell you about how important iron overload is, how common it is, and how important it is to handle this properly.
The way I heard about iron overload was through my wife, Laura. You can hear about her story here. To make a long story short, for years she suffered from what seemed to be immune system problems, hormonal problems, migrating joint pains, low energy, anxiety, and depression. Once she learned that she had iron overload, and started giving blood, about 90% of her symptoms went away. And she needed about 90% fewer supplements! Win! Thank God I listened to her when she asked me if she could have iron overload!
Just as importantly, however, I am telling you this so that you can see the difference between using the standard lab reference ranges and functional medicine blood chemistry reference ranges. If Donna, or my wife, Laura, had just used the standard lab reference ranges, both of them would most likely still be suffering today.
So, this begs the question, why don’t more doctors do this? The answer is simple, they are not trained in it. While they receive a tremendous amount of education on anatomy, physiology, pathology or disease, and pharmacology, they receive no training on functional medicine in medical school. It’s not that they’re doing something wrong, or making mistakes, they are just looking at health from a different perspective.
If this case interests you, and or you want to learn more about functional medicine, click here to learn more about our functional medicine program.
Yours in health,
Dr. Sheehan
Related Articles
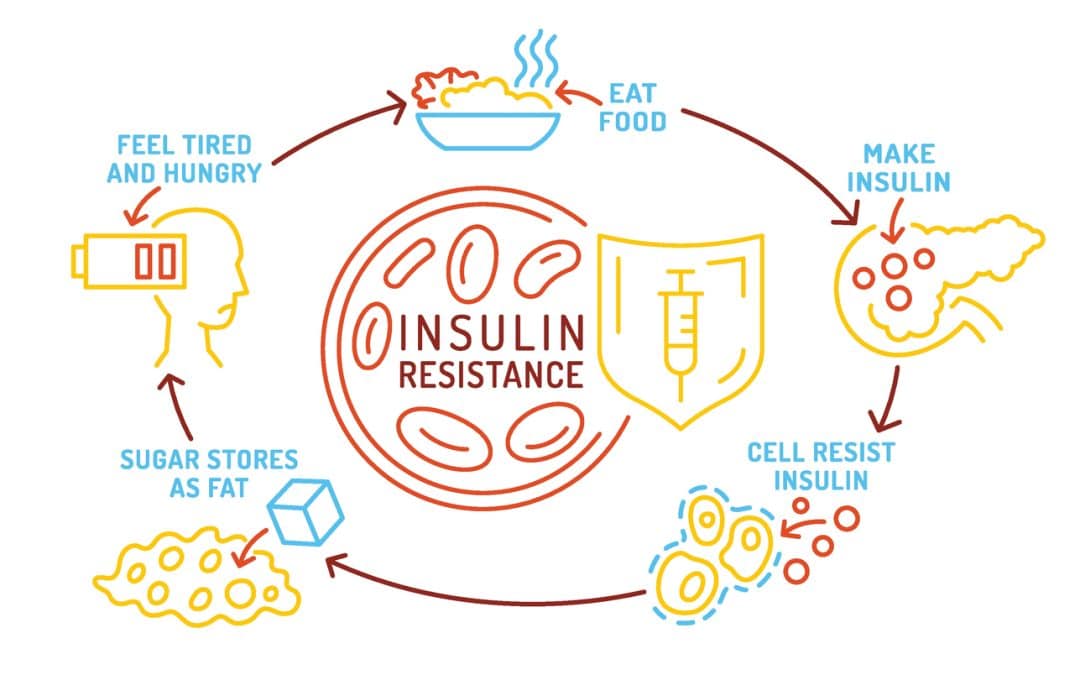
Insulin Resistance Explained: Early Signs, Functional Testing, and Natural Solutions
One of the things we talk about often in our office is a monster of a problem called insulin resistance—and for good reason. It's one of the most common yet overlooked root causes of issues like fatigue, stubborn weight gain, brain fog, hormone imbalances, and more....
Proactive Steps to Improve Your Thyroid Health (Plus 6 Case Studies!)
Table of Contents1. Understanding Your Thyroid2. How Low Thyroid Function Affects the Body3. Reduce Your Exposure to Toxins4. Avoid Foods You Are Sensative To5. Support Your Immune System6. Optimize Your Liver and Gallbladder Function7. Rule Out Scar Interference8....
Not All Allergy Testing Is The Same: IgE and IgG Differences
Most doctors will run IgE tests to find any severe reactions to foods, such as breathing issues or hives. IgG tests show delayed, less severe reactions to foods such as eczema patches and/or stomach issues. Food sensitivities may be less severe, but they will wreck...
Standard Laboratory Tests for Sheehan Natural Health
Standard Laboratory Tests for Functional Evaluation This is a list of the standard laboratory tests that we order in our office. Each test included a procedure code so that the laboratory can recognize the test. To learn more about these tests, watch our "How To Read...

New Years Offer At Sheehan Natural Health
Merry Christmas and Happy New Year! Greetings from Dr. Sheehan and Laura! I hope you had a nice holiday season, spent some time relaxing with the family, and so on. Since both Laura’s and my family live out of state, we stayed here and concentrated on our hiking...
How to Figure Out If You Have Inflammation, and How Much
One of the things that we find all the time in our patients is that they have more inflammation than is healthy. If you look at current studies, and research articles on health, you will see that inflammation is a big part of just about all disease processes,...
How Do I Keep My Immune System Strong?
The most common question that we get here in the office these days is “how do I keep my immune system strong?” The answer is quite easy: cut out what weakens it and increase what strengthens it. Here's What Weakens The Immune System 1. Sugar Sugar comes in many forms,...

The Page Diet: The Most Effective Diet For Overall Health
What is the Healthiest Diet? If you have been a patient of ours, you probably know there are many dietary strategies that can work very well to get you healthier and feeling better. The best diets out there minimize or eliminate processed foods and stress regular...
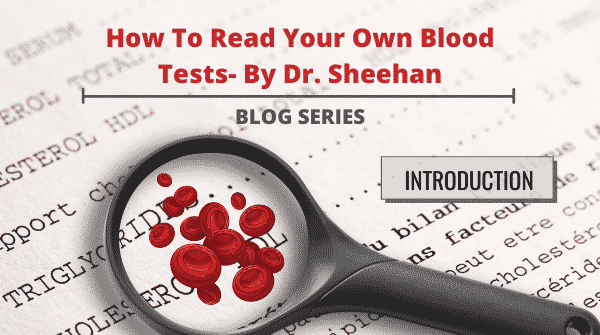
Dr. Sheehan Introduces His New Educational Series: How to Read Your Own Blood Tests
Recently, after taking a long hiatus from blogging and making videos to finish a side project on teaching doctors how to properly read blood tests, I realized I wanted to start blogging and making videos again. However, I wasn’t...

Is It Lyme Disease, Chronic Fatigue, or Something Much Easier?
7-year-old Female – Tired, Shy, Stomach Hurts When Regina came to see me in February, she looked like a healthy seven-year-old female. I asked her mother why she thought Regina needed my help. To which her mother replied “Regina always seems tired, really quiet, and...